Fidela Anne Salvador-Badiles, MD, Monica Therese Cating-Cabral, MD
Center for Diabetes, Thyroid and Endocrine Disorders, St. Luke’s Medical Center – Global City
A 54-year-old female with a history of hypertension presented in 2014 with dysuria, hematuria, polyuria, and urinary crystals. A urologist’s evaluation revealed nephrolithiasis and elevated ionized calcium levels, leading to Extracorporeal Shock Wave Lithotripsy (ESWL) treatment.

In 2017, a follow-up with her urologist revealed persistent hypercalcemia and elevated parathyroid hormone (PTH) levels, prompting a referral to endocrinology for suspected hyperparathyroidism. A parathyroid scan indicated increased tracer uptake in the inferior pole of the right thyroid lobe. Following a subtotal thyroidectomy and parathyroidectomy, histopathology confirmed a colloid goiter and parathyroid adenoma. Post-surgery, her calcium and PTH levels returned to normal.
In 2018, during a follow-up, the patient reported a milky discharge from both nipples and recalled experiencing symptoms since 2015: increasing hand and shoe sizes, numbness, and rings no longer fitting. She had paresthesias in both hands and was diagnosed with carpal tunnel syndrome, leading to bilateral release surgery in 2018. The patient noted the progressive nature of her symptoms but couldn’t recall their exact order of onset. She also mentioned multiple facial surgeries (2 blepharoplasties and 3 rhinoplasties) due to concerns about her nose enlarging. She denied experiencing headaches, tongue enlargement, tooth spacing, joint pain, fatigue, vision changes, or voice deepening.
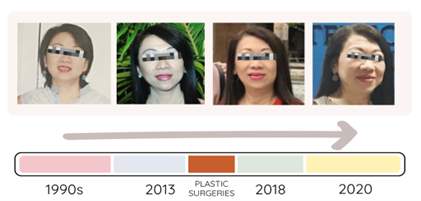
Figure 1. Transformation of patient’s facial features from 1990’s to 2020.
The patient presented with significantly elevated IGF-1 levels of 854 ng/mL and a dynamic GH test showing baseline and peak levels of 9.97 ng/mL to 11.55 ng/mL. A pituitary MRI revealed a 1.7 x 1.0 x 1.0 cm mass extending into the right cavernous sinus, encasing the right internal carotid artery. A colonoscopy identified colonic polyps. Mildly elevated prolactin at 82.69 ng/mL was noted (undiluted sample). A transsphenoidal excision of the pituitary tumor revealed a pituitary adenoma, positive for GH and prolactin on immunohistochemistry, with negative results for FSH, LH, TSH, and ACTH. A follow-up MRI after four years showed no tumor recurrence.
Should we evaluate for Multiple Endocrine Neoplasia Type 1 (MEN1) based on her presentation?



