Endocrine Causes of Hypertension by Gherald R. Bermudez, MD
Data from the World Health Organization as of 2019 showed an estimated 1.13 billion people living with hypertension worldwide. In our country, more than 12 million Filipinos are hypertensive.
Hypertension, or simply elevated blood pressure, is a serious medical condition that significantly increases the risk for stroke, ischemic heart disease, kidney failure, and other diseases. In fact, it is one of the top ten leading causes of morbidity and mortality both in our country and worldwide. It is diagnosed when, measured on two different days, the systolic blood pressure readings on both days exceed 139 mmHg and/or the diastolic blood pressure readings exceed 89 mmHg on both days.
Approximately 85% of all cases of hypertension is classified as idiopathic (primary or essential) or those with no identifiable secondary cause. A subgroup of approximately 15% have secondary or identifiable cause. Of these secondary causes, endocrine hypertension accounts for approximately 3% of all cases. Endocrine hypertension is a type of high blood pressure caused by hormone imbalance. There are at least 14 endocrine disorders for which hypertension maybe the initial clinical presentation. The most common causes of endocrine hypertension are excess production of mineralocorticoids (primary hyperaldosteronism), catecholamines (pheochromocytoma), thyroid hormones, and glucocorticoids (Cushing’s syndrome).

THYROID DYSFUNCTION, both hypothyroidism and hyperthyroidism, may increase the risk of hypertension. Hyperthyroidism occurs when there is an overproduction of thyroid hormones by the thyroid gland.
Because thyroid hormones accelerate the body’s metabolism, excess of thyroid hormones causes weight loss, rapid or irregular heartbeat and tremors. Other common signs and symptoms are weakness, hair loss, insomnia, protrusion of the eyeballs (exophthalmos), enlarged thyroid gland (goiter), sweating, irregular menses, and diarrhea.
Thyroid hormones also have direct and indirect effects on the cardiovascular system. These effects cause metabolic and hemodynamic changes leading to significant mechanisms causing increased cardiac output and increased blood pressure.
Hypothyroidism, on the other hand, occurs when there are not enough hormones produced by the thyroid gland. Common signs and symptoms are weight gain, easy fatigability, constipation, puffy face, heavy menses, hoarseness, muscle pains, slowed heartbeat, impaired memory, and goiter.
Hypothyroidism also increases blood cholesterol levels which may lead to atherosclerosis and hypertension.

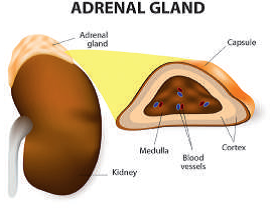
PRIMARY HYPERALDOSTERONISM is a hormonal disorder that leads to high blood pressure as a result of overproduction by the adrenal gland of a hormone called aldosterone. There are several important functions of the adrenal gland including the production of aldosterone which balances sodium and potassium levels in the blood.
Too much of this hormone causes the body to hold too much water, increasing blood volume and blood pressure. Usually, a high blood pressure, which is difficult to control, is the first symptom of this disease. Because an increase in aldosterone also causes a decrease in potassium level (hypokalemia), symptoms such as muscle cramps, weakness, headaches and fatigue may also be present.
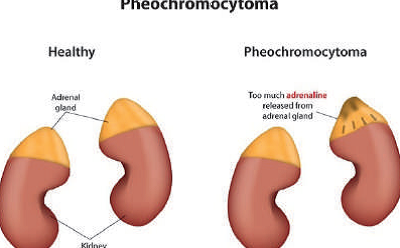
PHEOCHROMOCYTOMA is usually a benign tumor that originates in the adrenal gland. Normally, the adrenal glands also produce catecholamines that help many body functions including heart rate and blood pressure. Abnormal production of these hormones by a tumor causes episodic or persistent hypertension.
Patients with this condition manifest with high blood pressure, headaches, heavy sweating, palpitations, among other symptoms. These symptoms, typically known as ‘spells,’ are triggered when patients with this condition are under stress, physical exertion, surgery, or even labor and delivery, have taken foods like chocolate and cheese which are high in tyramine, and certain medications such as cocaine.
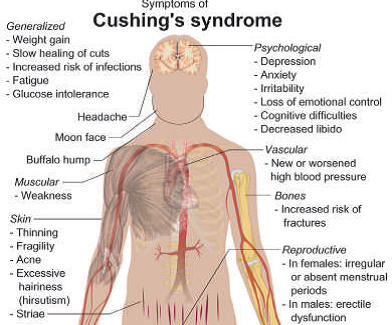
CUSHING’S SYNDROME occurs when the body is exposed to high levels of the hormone cortisol for a long time. This occurs when there is an overproduction of cortisol, a hormone which is normally produced by the adrenal gland, or an overproduction of adrenocorticotrophic hormone (ACTH), a hormone produced by the pituitary gland. ACTH is important for the regulation of cortisol. It may also be caused by intake of corticosteroids like prednisone, dexamethasone and methylprednisolone for a long time.
High levels of cortisol can produce some of the hallmarks of Cushing’s syndrome like moon facie, buffalo hump, and purplish stretch marks on the abdomen. In addition, Cushing’s syndrome can also result in hypertension, diabetes, and osteoporosis. If a patient is taking exogenous corticosteroids for a very long time and it is withdrawn abruptly, a life-threatening condition known as ‘adrenal insufficiency’ may develop; hence, intake of this type of medications should always be under the supervision of a physician.
Common signs and symptoms of Cushing’s syndrome, aside from those mentioned formerly, are weight gain, thinning of the skin resulting into easy bruising, acne, irregular or absent menses, appearance of visible body and facial hairs, weakness, infertility, depression, and fractures.
Although most cases of hypertension are classified as essential, it is important to consider other secondary causes especially when risk factors and common signs and symptoms are present. Treatment of endocrine causes of hypertension is directed to the cause of the abnormally produced hormone. It is important to consult an endocrinologist if and when an endocrine cause of hypertension is suspected.
References:
1. Berta E et al, Hypertension in Thyroid Disorders, Front Endocrinol. 2019; 10:482
2. Department of Health, Republic of the Philippines
3. Koch C et al, Overview of Endocrine Hypertension, Endotext. 2016
4. Shlomo M et al, William’s Textbook of Endocrinology, 13th ed. 2016
5. World Health Organization
Endocrine Causes of Hypertension by Gherald R. Bermudez, MD – Part of the March 2020 Endocrine Hotspots Edition
See our other Endocrine Hotspots Edition
Brought to you by the Philippine College of Endocrinology Diabetes and Metabolism (PCEDM)
Website: endo-society.org.ph
IG: @endocsociety
Twitter: @EndoSoc_ph
Facebook: fb.com/filipinoendocrinologists



