When Height is not Might: Acromegaly and Gigantis
Michelle Cornel, MD
What is the difference between Acromegaly and Gigantism?
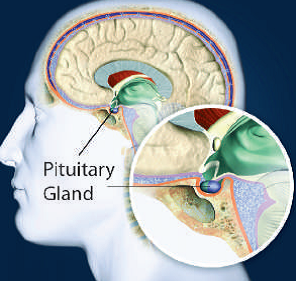
The pituitary gland located at the base of the brain produces several hormones, one of which is Growth Hormone (GH). GH is important in maintaining normal body structure and metabolism. Acromegaly is a rare disorder resulting from an excess production of GH in adults, occurring after the bones have stopped growing. In children in whom the bones are still growing, the excess in GH leads to Gigantism.
What are the causes?
The most common cause is a non-cancerous pituitary tumor that secretes excess GH. In very rare conditions, it can be caused by tumors outside the pituitary that secrete GH.
What are the signs and symptoms?
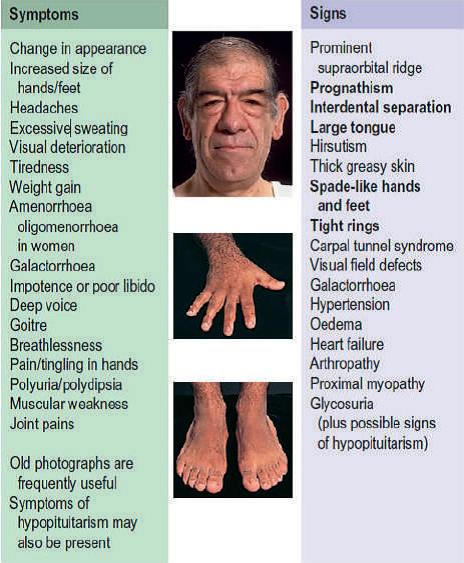
For adults whose bones have stopped growing, excess Growth Hormone (Acromegaly), usually presents as enlargement of hands and feet. Patients usually notice that their rings don’t fit their fingers anymore or that their shoe size is increasing.
They also might note changes in the shape of their face, such as widening of the spaces between their teeth or enlargement of their nose and thickening of the lips. Aside from these, they might observe that their lower jaw or brows might start to protrude or become more prominent. These changes often occur very slowly, so sometimes you can only see the differences when you compare the present with old photographs.
In children, who are still growing and have not yet reached their final height, too much growth hormone can lead to excessive growth of long bones. The end result is a child who is abnormally tall. However, other possible causes of tall stature should be evaluated, such as familial growth pattern and the child’s target height relative to his parents’ heights.
Doctors will have to evaluate if the child’s height is really abnormal based on their age and family background, as well as other factors. When there is family history of tall stature and no other signs and symptoms of gigantism are seen, and if the child has a normal growth rate, no further testing is needed.
As for the pituitary tumor itself, it may cause symptoms also if it compresses the nearby structures. These symptoms include headache and vision problems. The tumor may also affect other pituitary hormones, in which case the patient may experience abnormalities in menses, loss of sexual desire, or tiredness.
Anyone presenting with the above signs and symptoms should consult an endocrinologist.
What are the other associated conditions?
Since GH also affects soft tissue growth and metabolic function, other conditions may occur such as the following:
– Hypertension (increased blood pressure)
– Diabetes (increased blood sugar levels)
– Heart disease – Osteoarthritis
– Sleep apnea (breathing repeatedly stops during sleep)
– Colonic polyp
– Goiter (enlargement of thyroid gland)
Monitoring of the occurrence of these conditions is important among patients with increased GH secretion.


How is Acromegaly or Gigantism diagnosed?
Upon consultation, patients presenting with suspicious signs and symptoms may be asked to do a 75-gram oral glucose tolerance test (OGTT). Their blood Insulin-like Growth Factor -1 (IGF-1) levels will also be checked.
What is the OGTT? In this test, blood glucose and GH are measured after 8 to 10 hours of fasting. The patient will then be asked to drink 75 grams of a very sugary drink, after which blood will be extracted to measure GH and blood glucose after 30, 60, and 120 minutes. If the GH does not decrease to less than 1 ng/ml during the test, it is highly suggestive of GH excess.
IGF-1 is a hormone that is closely related to growth hormone. GH, when released, stimulates the liver to produce IGF-1. In the blood, IGF-1 levels have less fluctuations throughout the day as compared to GH levels. That’s why elevated values relative to a person’s age and sex are indicative of GH excess.
Once a patient has been diagnosed to have too much GH, imaging tests are needed to localize the site of the excess production. A pituitary MRI is usually requested to check for the presence of a tumor, which accounts for 95% of cases of Acromegaly and Gigantism. When this MRI does not show a pituitary tumor, then a CT scan of the abdomen or chest is warranted to check for the presence of any nonpituitary GH-secreting tumor.
What are the treatment options?
If the cause of Acromegaly or Gigantism is from the pituitary tumor, surgical removal of the tumor is recommended. Following surgery, regular follow up with monitoring of blood IGF-1 and GH is done.
Medical therapy is recommended for patients with persistent disease despite surgery.
Radiation therapy may be appropriate for patients with residual tumor after surgery. This may also be an option if medical therapy is unavailable, unsuccessful or not tolerated.
Based on the patient’s condition and diagnostic test results, and after discussion of the benefits and the side effects of each treatment option, the endocrinologist and the patient can then reach a decision regarding the most appropriate therapy.


Why is proper treatment important?
Patients with uncontrolled GH levels often develop diabetes, hypertension and heart disease. They may also develop tumors in their large intestines. More than that, their life expectancy may be reduced by approximately 10 years. In order to avoid these complications, appropriate treatment is necessary. Those patients who are successfully treated and who achieve normalization of their IGF-1 and GH can then anticipate a normal life expectancy.
REFERENCES:
Acromegaly retrieved from https://www.hormone.org/diseases-and-conditions/acromegaly
Diagnosis and Treatment of Excess Growth and Tall stature, Williams Textbook of Endocrinology 12th edition
Acromegaly: An Endocrine Practice Guideline retrieved from
https://academic.oup.com/jcem/article/99/11/3933/2836347
Part of the March 2020 Endocrine Hotspots Edition
See our other Endocrine Hotspots Edition
Brought to you by the Philippine College of Endocrinology Diabetes and Metabolism (PCEDM)
Website: endo-society.org.ph
IG: @endocsociety
Twitter: @EndoSoc_ph
Facebook: fb.com/filipinoendocrinologists



