Maria Nikki Cruz MD, Noemi Nunez MD,
Aaron Perez MD, Michael Rosario MD
CASE

Patient is a 70-year-old male, non-hypertensive, non-diabetic, who was referred for evaluation of hypercalcemia.
History started 9 years prior, when patient had lumbar pain, non-radiating, not triggered by movement, with no associated symptoms. He sought consult with a nephrologist, and KUB x-ray showed a right pelvic calcification suggestive of a phlebolith. KUB ultrasound showed normal-sized kidneys with cyst wall calcification or non-obstructing calyceal lithiasis, left with consideration of medullary nephrocalcinosis bilateral. He was referred to a urologist and underwent extracorporeal shock wave lithotripsy. Further work-up showed elevated iCa 1.41(NV 1.09-1.30mmoL/L) and iPTH 73.40(NV 15-65pg/mL). Parathyroid sestamibi scan did not show any avid focus. No further intervention was done.
During the interim, patient remained asymptomatic. 7 years prior, laboratory work-up revealed elevated iPTH 82.22 pg/ml and creatinine 1.47 mg/dl (EGFR 47), normal total calcium 9.2 mg/dL, and low phosphorus at 2.4(NV 2.5-4.9mg/dL). 24-hour urine calcium was normal at 0.170(NV 0.1-0.3 g/24hrs). No further evaluation done. iPTH was noted to be persistently elevated with normal calcium levels; hence, parathyroid sestamibi scan was repeated 2 years prior, which showed a suspicious sestamibi-avid focus in the lower pole of the right thyroid lobe, possibly indicative of a parathyroid adenoma. He was assessed to have primary hyperparathyroidism secondary to parathyroid adenoma and referred to an endocrinologist for further evaluation. Neck ultrasound showed a well-defined extrathyroidal hypoechoic nodular structure, measuring 0.5×0.6×0.6 cm. However, repeat laboratory work-up revealed elevated iCA 1.39 mmol/L, a high normal iPTH 77.9 pg/ml and a normal Vitamin D 31.2 (NV 30-80 ng/ml). Repeat 24-hour urine calcium was low at 0.051 g/24hrs. Bone densitometry revealed osteopenia (-2.1). He was then assessed to have familial hypocalciuric hypercalcemia.
The patient had no family history of kidney stones, thyroid disease, or type 2 diabetes mellitus. Patient consumes soda, but no intake of calcium supplements. He was a previous smoker and alcoholic beverage drinker.
DIAGNOSTICS
Table 1. Summary of laboratory results
| DATE | iPTH | iCa (NV 1.09-1.30mmoL/L) | P (NV 2.5-4.9mg/dL) | Viatmin D total(30-80ng/mL) | Creatinine (NV 0.7-1.3mg/dl) |
| 2014 | 73.40(NV 15-65pg/mL) | 1.41 | 1. 1.31 | ||
| 2016 | 82.22 | 2.4 | 1.44 | ||
| 2018 | 101 | 1.6 | |||
| March 2021 | 108.50 | 1.39 | 1.34 | ||
| August 2021 | 77.9 | 1.39 | 2.3 | 31. | 1.24 |
| 2/14/22 | 87.9(NV 18.5-88 pg/mL) | 1.39 | 2.6 | 34.83 | |
| 9/7/22 | 79 | 1.34 | 2.8 | 42.09 | |
| 11/10/22 | 101.70 | 1.31 | |||
| 4/10/23 | 95.40 | 1.30 |
Figure 1. Sestamibi imaging showing a suspicious Sestamibi-avid focus in the lower pole of the right thyroid lobe may be due to a parathyroid adenoma
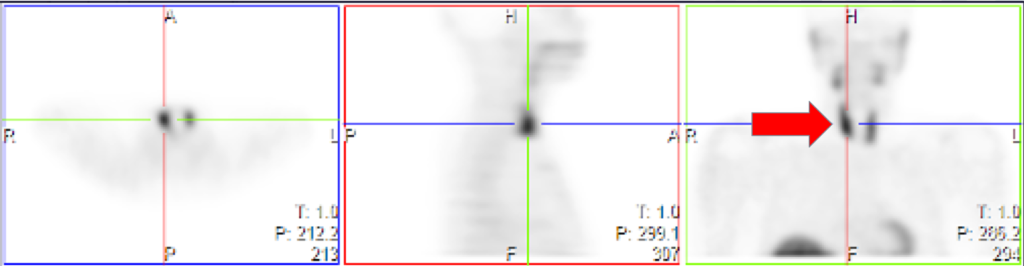
Figure 2. Neck ultrasound showing right posterior thyroid region demonstrating a well-defined extrathyroidal hypoechoic nodular structure measuring approximately 0.5 x 0.6 x 0.6cm suggestive of parathyrid adenoma

CLINICAL DILEMMA
- What is your diagnosis?
- If Familial Hypocalciuric Hypocalcemia is considered, how do we treat the osteopenia in a 70 year old male with a slightly elevated iPTH, normal to slightly high calcium and normal Vitamin D?
- When do we address the parathyroid adenoma seen on the Sestamibi scan?



