Kurt Bryan O. Tolentino, MD, Maria Patricia Deanna D. Maningat – Goco, MD
Center for Diabetes, Thyroid and Endocrine Disorders
St. Luke’s Medical Center – Global City
Papillary thyroid carcinoma still remains to be the most common thyroid malignancy occurring in approximately 4.8 to 14.9 per 100,000 patients,1 but often does one see this malignancy coexist with another rare endocrine disorder? Coexistence of this malignancy to various tumors has been reported to be associated with other syndromic disease entities, however, it’s association to an isolated central hypothyroidism from a pituitary macroadenoma remains to be seen. We explore a case of a patient with an enlarging anterior neck mass where upon further workup revealed an isolated hypofunctioning pituitary tumor.

This case reports a 67-year-old female, known prediabetic and hypertensive, with an anterior neck mass that started 30 years prior to consult, initially approximately 1×1 cm in size with no other associated symptoms. She did not opt to seek consult during this time. In the interim, she noticed that the mass was gradually increasing in size.
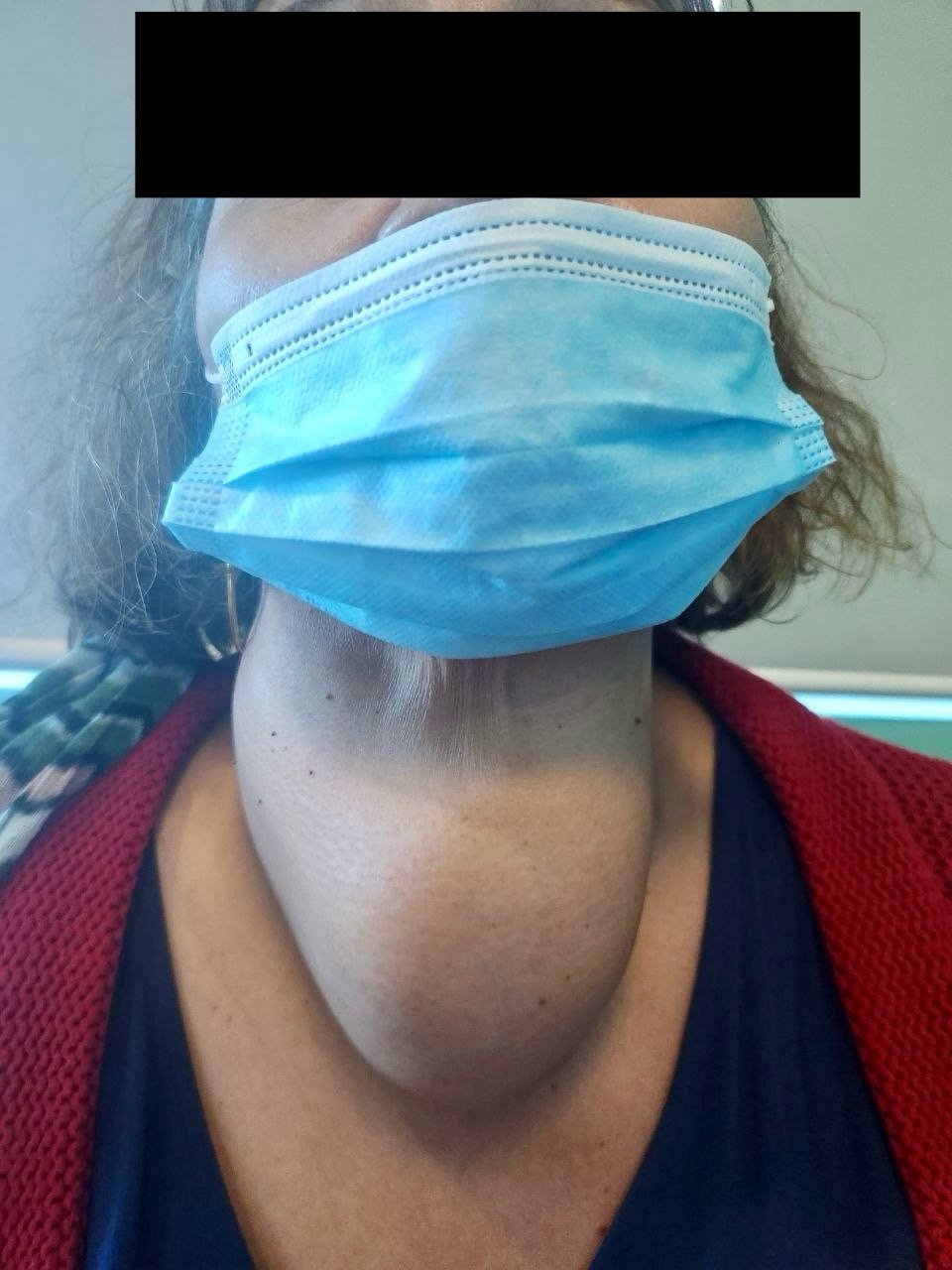
One year prior, due to the persistence of enlargement of her anterior neck mass, now with easy fatigability, she sought consult with her attending medical doctor where work up done showed a normal thyroid function test including a TSH of 0.56 uIU/mL (0.27-4.20) and a FT4 of 0.77 ng/dL (0.93-1.71). Thyroid ultrasound done showed a heterogenous echopattern (solid w/ cystic areas) in both lobes and isthmus region. An ill-defined heterogenous solid area measuring 1.8 x 3.3cm is noted in the inferior aspect of the right lobe. Ill-defined hypoechoic-hyperechoic solid areas, the largest measuring 1.9 x 2.8cm, were seen scattered in the left lobe with calcifications noted in both lobes. CT scan of the neck was subsequently done showing a heterogenous enhancing mass with calcifications at the right thyroid bed 9.3 x 11.4 x 12.9cm with a volume of 715ml, with noted compression of adjacent structures.
She was advised to undergo a surgical intervention prompting further evaluation by a cardiologist. A repeat thyroid function test done after 6 months revealed a low FT4 11.32 pmol/L 12.0-22.0) and TSH 0.021 uIU/mL (0.27-4.20) and a normal FT3 8.84 pmoL/L (2.8-7.1). She was prescribed Levothyroxine 50mcg once daily and advised repeat thyroid function tests after 1 month revealing persistence of low TSH 0.038 uIU/mL and FT4 0.68ng/dL (0.89-1.76).
On follow up, she did not complain of vision changes, dizziness, headache, cold intolerance, constipation or any other symptoms. Due to the persistence of these low laboratory findings, she was advised to undergo a pituitary MRI, which revealed a 9 x 12 x 9mm hypopenhancing, pre-existing T1-W and T2W hyperintense nodule superior to the adenohypophysis and posteriorly displacing the infundibulum. The nodule also mildly abuts the left optic nerve. The pituitary stalk is midline. Optic chiasm not affected. Cortisol and Prolactin levels were tested revealing normal results.
She continued Levothyroxine supplementation, referred to ENT service, and was advised to undergo thyroidectomy. She was sent home well with no complaints. Histopathology results revealed papillary thyroid carcinoma, follicular variant, infiltrative, right lobe (18.5 cm) with an atypical follicular lesion at the left lobe (1.5 cm). No extrathyroidal extension to skeletal muscle and subcutaneous fat was noted but lymphovascular invasion was present. There were no perineural invasion. The carcinoma was within 1 mm of nearest inked margin.
There have been no reports on the occurrence of the coexistence of a pituitary macroadenoma with isolated central hypothyroidism and papillary thyroid carcinoma. This can be from the extremely rare occurrence of central hypothyroidism ranging from 1 in 80,000 to 120,000 individuals.2 There have been no case reports cited with these 2 disease entities occurring at once, however, reports of metastatic lesions of papillary thyroid carcinoma have been reported, mostly showing signs of mass effect and central hypothyroidism as well, where management involved surgical removal of the pituitary mass.3
Moreover, since treatment of this case requires the use of radioactive iodine therapy due to its high risk features, the lack of an increase in TSH due to central hypothyroidism poses a challenge to increase the said hormone. Could the use of recombinant TSH (rhTSH) be an alternative to increase the TSH of this patient in preparation for RAI therapy? Case studies from previous cases include patients diagnosed with papillary thyroid carcinoma in patients with panhypopituitarism. All of these cases were given rhTSH 0.9mg once daily for 2 days with an interval of 24hrs. A repeat whole body scintigraphy showed no pathologic tracer activity with low serum thyroglobulin and anti-thyroglobulin concentrations.4 This can be considered to our patient in the future.
Literature for this case remains to be seen, however, the occurrence of low TSH and FT4 merits the evaluation of the pituitary gland via MRI for further evaluation and appropriate management for these cases. Recombinant human TSH can be an alternative to raise TSH prior to radioactive iodine treatment to treat intermediate to high risk patients with central hypothyroidism.
REFERENCES:
- Limaiem F, Rehman A, Anastasopoulou C, et al. Papillary Thyroid Carcinoma. [Updated 2023 Jan 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from:https://www.ncbi.nlm.nih.gov/books/NBK536943/
- Gupta, V., & Lee, M. (2011). Central hypothyroidism. Indian journal of endocrinology and metabolism, 15(Suppl 2), S99–S106. https://doi.org/10.4103/2230-8210.83337
- Butt, M. I., Siddiqi, A. M., & Joueidi, F. M. (2023). Papillary Thyroid Cancer With Pituitary Gland Metastasis: A Unique Encounter. Cureus, 15(4), e38210. https://doi.org/10.7759/cureus.38210
- Topaloğlu Ö et al. Difficulty in follow-up of papillary thyroid cancer co-existent with hypopituitarism: case report and review of the literature. Med J West Black Sea. 2022;6(3):410-416.



